In Rajasthan, mining is second only to agriculture. There are 42 major minerals and 23 more minor ones extracted here, and roughly 2 million mine workers statewide. But while mining is big business, it isn't very modern. Many mineworkers still labour in the same awful conditions as their predecessors did decades ago, and earn only a pitiful amount, around Rs.40 daily. Their exposure to occupational hazards such as respiratory ailments remains very high, and ailments such as asthma, tuberculosis and silicosis are common. Silicosis is the most fatal of these, and one of the main causes of deaths among mineworkers in Rajasthan.
Silicosis develops over time when dust-containing silica is inhaled repeatedly into the lungs. Large amounts of organic dust particles (their sizes vary from 0.1 micron to 150 microns) exist in mines, and smaller particles (smaller than 5 microns) may become airborne and respirable. When the dust of the mines is inhaled, silica particles end up in the air sacs of the lung. The body's defence system quickly attacks the silica particles, releasing enzymes and radicals. The release of these by-products can result in death of lung tissues and white blood cells, which causes inflammation. The inflammation and scarring that damages the lung sacs prevents gas exchange and normal breathing. Damage to the lung tissue means that the capacity of the lungs to supply oxygen to the blood is reduced.
The disease progresses in three stages. During the first stage, the patient feels some difficulty in breathing, has a mild cough and sputum production. During the second stage, in addition the patient complains of chest pain and reduced work capacity. During the third stage, the disease becomes life threatening. The patient becomes almost helpless, and symptoms like severe cough, bloodstained sputum, continuous chest pains and rapid weight loss become very prominent, eventually leading to premature death. Without these signs, silicosis can be difficult to diagnose; nodules that collect to form a mass can take up to 20 years to be identified in chest x-rays. The victim thus notices the symptoms only after several years of exposure, nor is there treatment for the disease only diagnosed.
Prevalence of the disease
A number of studies carried out in mining areas and related fields point in the same direction: incidence of silicosis is high among mineworkers and communities neighbouring the mines. Surveys conducted by Indian Council of Medical Research (ICMR) have reported rates between 16-57 percent in different parts of the country. In another study by Prof. PK Gupta and his associates at the department of Chest Diseases of Dr. SN Medical College, Jodhpur, radiological investigations of 82 mineworkers were carried out. The report of the investigation suggests that 56 percent of the mineworkers were affected with silicosis or silica-tuberculosis.
![]() Gramin Vikas Vigyan Samiti (GRAVIS), a Jodhpur based NGO, in collaboration with Society For Participatory Research In Asia (PRIA), Delhi have performed two independent surveys among mineworkers in the [WHICH] district of Rajasthan. The first was a study in 1994, which found that about 10% of the mineworkers examined suffered from silicosis. A second study was conducted in 1996, when GVVS and PRIA conducted another elaborate medical examination among the mineworkers at the sandstone mines in Jodphur. In addition to the Lung Function Test, chest X-rays were also taken of all the workers to screen for any related radiological abnormalities. Out of the 288 workers examined, 14% were found to be suffering from severe silicosis, and 28% were found to be suffering from silicosis of less severity. If these numbers are indicative of mines throughout the state, then up to 800,000 workers might be affected.
Gramin Vikas Vigyan Samiti (GRAVIS), a Jodhpur based NGO, in collaboration with Society For Participatory Research In Asia (PRIA), Delhi have performed two independent surveys among mineworkers in the [WHICH] district of Rajasthan. The first was a study in 1994, which found that about 10% of the mineworkers examined suffered from silicosis. A second study was conducted in 1996, when GVVS and PRIA conducted another elaborate medical examination among the mineworkers at the sandstone mines in Jodphur. In addition to the Lung Function Test, chest X-rays were also taken of all the workers to screen for any related radiological abnormalities. Out of the 288 workers examined, 14% were found to be suffering from severe silicosis, and 28% were found to be suffering from silicosis of less severity. If these numbers are indicative of mines throughout the state, then up to 800,000 workers might be affected.
Laws and enforcement
The potential hazards from silicosis have been known for a long time, and a number of state governments have passed legislation to address this. On the basis of a coal mining report, silicosis was first made noticeable under the Factories Act. Under the Workmen Compensation Act 1923, the Rajasthan Silicosis Rules, 1955 were established. A decade later, the government came out with the 'The Rajasthan Workmen's Compensation (occupational diseases) Rules, 1965 in exercise of its power under Section 32 of the Workmen's Compensation Act, 1923 . These new Rules of 1965 came into force with effect from September 20, 1965 of that year, and these define afresh the Occupational Diseases under various classes; Pneumoconiosis - which covers Silicosis or Coal Miners Pneumoconiosis or Asbestosis or any of these disease accompanied by Pulmonary tuberculosis - was mentioned under one of these classes.
Rule 4 of the rules promulgated in 1965 also provides for the establishment of a Pneumoconiosis Medical Board. This board would conduct medical examinations, submit medical reports and grant medical certificates to workmen employed in mines. But the government did not act promptly to constitute this board - an all-too-familiar example of the administrative machinery simply being disconnected from the law. Finally, in 1993, twenty eight years after the notification, the Department of Labour of the Government of Rajasthan constituted the Pneumoconiosis Medical Board in 1993 with three doctors.
These developments, anyhow, meant nothing in practice; to date, no person affected with Silicosis has ever received any compensation or reimbursement of costs of treatment by the court orders in Rajasthan. Besides the fact that almost none of the mineworkers are aware of the regulations and laws, the procedure for filing a compensation petition is very complicated. The biggest hurdle in the whole process is the difficulty in obtaining a certificate from the Pneumoconiosis Board. With the board inordinately delayed - and even then largely idle - actual relief for the mineworkers remains out of reach.
There are other rules, equally breached. Rule 9 of the Silicosis Rules (1955) requires every employer before hiring any new worker to present this worker before a medical practitioner for medical examination. Only after issuance of Certificate 'C', the worker will be employed. The Rule further provided a check-up after every 5 years when requirement of Certificate 'B' is necessary, to prove that the worker is not suffering from Silicosis, or Certificate 'D' for the worker who is suffering from Silicosis. The rules provide ample provisions but no such examination has ever been carried out. Rule 10 of the Silicosis Rules, 1955 provides for post mortem examination to establish if the deceased workman's heirs are eligible for compensation. However, no medical practitioner is authorised by the Government to do the examination and no proper procedures are laid for the procedure - another example of incomplete - and thus shoddy - lawmaking. The rules thus remained dead letters.
HEDCON's action on behalf of mineworkers
Then the Health, Environment, and Development Consortium (HEDCON, an NGO in Rajasthan) decided to engage this struggle; it began by looking at the activities of the Pneumoconiosis Board. In 2003, HEDCON found that this board was dysfunctional because of vacant posts of board members. The issue was raised during a journalists' workshop on 10th February, 2003, leading to many news items published by newspapers in Rajasthan. Next, from March 2003 onwards, HEDCON corresponded with various departments, as well as political and administrative leaders - the Chief Minister, other Ministers, the Chief Secretary, and Secretaries of the Pollution Control Board, the Medical and Health Department and the Labour Department. Written communication was also taken up with State Human Right Commission. A notice for demand of Justice regarding the non-functioning of the Pneumoconiosis Medical Board was issued. To this, HEDCON never received any reply from the State Government. On 4 December 2003 a Public Interest Litigation was filed in the High Court; the two-judge bench issued a notice to related departments to present their views on the matter on 23rd January, 2004.
As the pressure grew, the government responded, and the Labour Department acted to reconstitute the Pneumoconiosis Board. A survey on Tuberculosis was organised by the Medical and Health Department in mining area in Jodhpur. The Labour Department was also directed to make required changes in the Workmen's Compensation Act to make it easier for mineworkers to obtain compensation through the courts. These developments, however, remained superficial; the improvements in safety, certification, monitoring, and compensation procedures that were promised never materialised. When questioned, Dr. N K Jain, the Chairperson of the Board, responded that the role and duties of the body still needed to be clarified; this explanation was also offered by Dr. Jain to the State Human Rights Commission, which responded to a case filed before it by HEDCON.
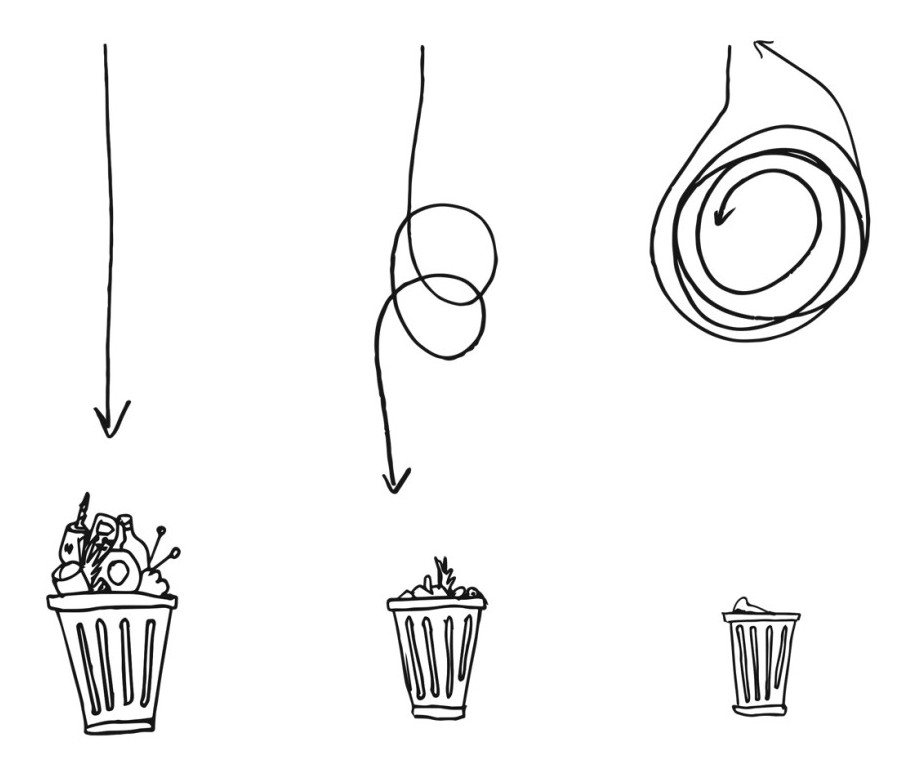
The quest for justice meandered around and eventually, the office of the Labour Commissioner - which too had initially turned away claims for compensation - agreed to take the cases. Within two months, 19 compensation cases from Silicosis patients were filed with the Labour Department. This development too proved illusory; after about a month, all the cases were thrown back, and we were told that without the certification of the Board, the Labour Court would not accept the cases. The circle of despair had come around - our efforts to get the Board to do its job was now both the starting point and the end of the search for justice.