In January this year, Dr R K Gupta was honoured by the Government of Chhattisgarh for performing 50,000 laparoscopic tubectomies. 10 months later, he was arrested under charges of causing death by negligence in the same procedure he was once lauded for. On 10 November, Gupta defied government medical protocol and conducted 83 laparoscopic tubectomies in just five hours in a mass sterilisation camp organised by the Government of Chhattisgarh. This fateful stint left 13 women dead and many others battling for their lives.
Two weeks since the tragedy, during which the people saw the usual blame game playing out between the Government of Chattisgarh, the practitioner and the pharmaceutical company supplying the medicines, a drug sample report has confirmed that the medicines given to the victims did indeed contain poisonous substances, zinc phosphide or rat poison being one among them.
Clearly, there is a much larger issue concerning the health industry in India, that has been brought to the fore one more time and which remains largely unaddressed despite various concerns raised earlier.

Pic: Wikimedia
Understanding drug adulteration
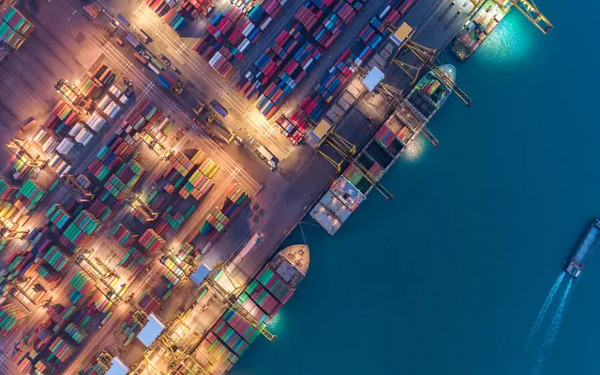
India is considered one of the most proliferating markets for counterfeit drugs. India's pharmaceutical industry ranks fourth in the world in terms of production volumes and over 55 per cent of its exports are to highly regulated markets, as a paper by Saurabh Verma, Rajender Kumar and P.J. Philip points out.
The menace of counterfeit drugs is not a new one. According to information on counterfeit drugs put out by the World Bank, the appearance of such medicines in international trade and commerce was first mentioned as a problem at a World Health Organization (WHO) Conference of Experts on Rational Drug Use in Nairobi, Kenya, in 1985. Eventually, more countries started openly acknowledging the increasing market of counterfeit drugs.
Despite the booming business of counterfeit drugs, according to WHO, there has been no agreement among countries on what constitutes a counterfeit drug. The most widely accepted definition is the one developed by WHO itself which defines a fake or a counterfeit drug as a medicine deliberately and fraudulently mislabelled with respect to identity and/or source.
Counterfeiting can apply to both branded and generic products and counterfeit products may include products with the correct ingredient, with the wrong ingredients, without active ingredients, with insufficient active ingredients or with fake packaging (WHO, 2005). Generally, all counterfeit drugs are substandard but a substandard drug may not be considered as counterfeit if there is no intent to deceive (Reggi, 2007).
A 2014 paper published by the Associated Chambers of Commerce & Industry of India (ASSOCHAM) titled “Fake and Counterfeit Drugs in India - Booming Biz” says that fake drugs constitute a staggering US$ 4.25 billion as against the total of US$ 14-17 billion of the domestic drugs market!
A slightly older report published in 2003 by ACG Worldwide stated that 75 per cent of counterfeit drugs supplied the world over can be traced back in one way or the other to origins in India, followed by 7 per cent from Egypt and 6 per cent from China.
These low-quality, spurious drugs are usually sold at sub-standard rates for those who cannot afford quality healthcare and medicines. In a developing country like India, a large population depends on these inferior, cheap drugs for some respite, thereby increasing the demand for the same.
A safe haven for unsafe drugs?
The ASSOCHAM study states that the thriving business of fake drugs is perpetuated by a lack of adequate regulations, shortage of drug inspectors and a lack of lab facilities to check the purity of drugs. India’s status as a low cost manufacturing base has opened up the gates for counterfeiters.
Counterfeiters share none of the heavy research and development costs incurred by genuine manufacturers, and yet are able to earn high profits, writes Verma et al. in the paper referred to above. Other key factors cited by the authors include storage of spurious drugs by the chemists, weaknesses in the drug distribution system, pricing of drugs, lack of awareness among consumers and the cost and complexity of identifying counterfeit or sub-standard drugs.
“Consumers, and sometimes prescribing physicians themselves, cannot tell the difference between the legitimate product and a counterfeit one. For example, if a patient consumes the fake, but recovers naturally, there is no reason to suspect a counterfeit product. Drug counterfeiters are growing more and more sophisticated by using latest technology systems in their illegal business,” specifies the paper.
Stressing the element of weak regulation, renowned economist and former chairman of the Institute for Social and Economic Change in Bangalore, S L Rao says, “Small scale units producing pharmaceutical products, poor regulation, inadequate inspection of drugs manufacture, and zero inspection of doctors and their prescriptions have all contributed to this menace.”
Rao feels that the blame rests squarely on the government that has allowed manufacturers, doctors, hospitals and retailers to make and sell sub-standard and fake drugs, and to sell drugs beyond the date of expiry. “Drugs are essential for patients who go and get them because their doctor has told them to. The really-poor buy such drugs from illegal and unlicensed quacks who keep stocks. Neither they nor the manufacturer face any regulation,” he points out.
In India, the task of regulating drug manufacture and sale rests with the State Licensing Authorities appointed by the state governments. The state governments appoint drug inspectors who, in their assigned areas, are required to inspect all establishment licensed for manufacture or sale, to make sure that the conditions of the licence are being followed. This well-chalked out system however, is not effectively utilised.
An article by Rao published in the Economic Times in 2004 articulated in detail the functioning of the counterfeit industry. “Our drug regulatory system is good only on paper. It is grossly understaffed, underpaid, under-equipped and under-skilled. The lawbreakers are extremely well financed and use their tax-free criminal earnings to buy co-operation. Our governance system is easily manipulated. Trials are slow, laboratories are slow and sloppy, evidence is lost, police officials change, witnesses are easily 'persuaded' to change their stories and prosecutors help the prosecuted,” Rao had written in that article.
10 years after the article was published, the conditions haven’t improved says the author. “The regulation of manufacturers, the ineffectiveness of the Medical Council of India in regulating prescriptions by doctors, the failure of the drug control authorities in states to stop retailers from giving dangerous drugs to anyone who pays, without prescription, are still to blame,” Rao adds.
The Pharmaceutical Security Institute (PSI) discovered 2193 incidents of pharmaceutical crime during 2013 alone. Piyush Misra from the Partnerships for Safe Medicines states, “The biggest challenge is lack of enforcement of the law (Drugs & Cosmetics Act, 1940) by the State Government, which is mainly due to inadequate infrastructure, untrained personnel and poor regulatory oversight.”
An amendment bill to the Act was drafted in 2008 after a 2003 committee report suggested death penalty as punishment for offenders. The bill sought to provide penalties for the manufacturer of spurious and adulterated drugs which would be “punishable with imprisonment of a term which shall not be less than 7 years but which may extend to imprisonment for life and with fine which shall not be less than 3 lakh rupees or three times the value of the drugs confiscated, whichever is more”. The bill however continues to be stuck in the Parliament.
The figures relating to the counterfeit drug market meanwhile continue to shock. According to the ASSOCHAM report, the fake drug market in India is currently growing at 25 per cent. If this spur continues, it will cross the US$ 10 billion mark by 2017. Despite such staggering figures, however, the physical existence of the counterfeit industry in India remains shadowy and is yet to be mapped.
The need for an awakening
Denial may also, in part, be to blame for this sustained threat. The Government of India conducts an “All India Survey” to determine the extent of spurious and below par (not-of-standard-quality) drugs in India. The survey, last conducted in 2009, studied 24,000 samples across the country and concluded that the extent of spurious drugs in the country was an absurdly low 0.046 per cent.
In September 2014, the government made an announcement that it will be conducting a fresh survey in 2014 in association with Central Drugs Standard Control Organisation (CDSCO) and the Indian Statistical Institute and other partners, including the state drug controllers. One hopes that this survey will provide better insight into the counterfeit industry today.
However, any survey can only help in determining the extent of the problem. What we need is a systematic plan to target the problem at its roots: stricter laws and regulatory bodies, effective distribution channels, and an urgent need to educate the consumers about the perils of such drugs.
REFERENCE: The Business of Counterfeit Drugs in India: A Critical Evaluation