In the last century, penicillin was the wonder drug. In India, it was one of the most potent drugs to fight bacterial infections that otherwise killed thousands of young children every year. Penicillin was used to treat pneumonia, meningitis and sepsis. But these days doctors are worried that penicillin is becoming less and less effective, as bacteria have learned to battle it.
The Invasive Bacterial Infectious Surveillance (IBIS) programme was begun in 1993 to track how bacteria are responding to common drugs, and to help us understand the resistance patterns that were emerging in the country. Dr. Kurien Thomas, Director of Clinical Epidemiology at the Christian Medical College, Vellore, is the programme's principal investigator. He says, "When IBIS was started, no resistance to penicillin was seen. But intermediate resistance was seen in 1998. And it has been gradually increasing since then."
The World Health Organisation too confirms that pneumococcal infections are becoming difficult to treat, as bacteria are turning more resistant to commonly used antibiotics. For example, the widely consumed antibiotic, cotrimoxazole (sold under the brand name Septran) was found to be no longer effective, due to resistance developed by the bacteria. It is used for all kinds of upper respiratory infections, but in 85 per cent of the cases, bacteria are able to resist the drug.
The mortality rate in hospitals of patients suffering from severe pneumonia ranges from three to five per cent. But more shocking is the mortality rate due to meningitis - that is between 35 and 50 per cent. At times, children end up with their limbs paralysed.
Even when properly used, drugs gets into the environment and in due course the bacteria will develop resistance to them. But oversue of antibiotics hastens the process, forcing us to keep coming up with new drugs every few years.
Dr. Thomas point out, for example, that the misuse of penicillin compounds has led to the development of resistance to penicillin. The resistance to penicillin was waiting to happen. It was carelessly used in veterinary care, increasing its presence in the environment. Now, the only recourse left to doctors attending young patients with bacterial infections is to prescribe cephalosporin, a third-generation alternative that is expensive. The danger now is that the bacteria will become resistant to the new drug too. Then a fourth generation drug will have to take its place, and that will not only be even more expensive but more toxic too.
India does not have an antibiotic policy that can regulate its use, and this complicates things further. There can be no strategy to stem the growth of Superbugs until the country first has reliable data.
Careless use of chemicals in agriculture has been shown to aggravate the bacterial resistance problem. India is today the largest producer and user of pesticides. Many of them are banned in the rest of the world.
•
Sitting on an epidemic
•
Will PHFI be meaningful?
•
TB, the gravest danger
The frontline illnesses
Nowhere is the problem more evident than in treating tuberculosis. "India's main problem is tuberculosis, as the TB germs are getting immune to conventional medicine, which today is a mixture of five drugs. It has a course of around six to nine months. Many patients stop taking the expensive drugs once they feel better and so the TB bacteria develop immunity. It is very difficult to treat Extremely Drug Resistant TB that is increasing everyday," warns Dr. Ramachandran, professor of microbiology at the University College of Medical Sciences in Delhi.
In India, every minute someone somewhere dies of TB in India. But it is not making national headlines. The Tuberculosis Control Board of India warns that treatment of Multidrug-resistant Tuberculosis (MDRTB) requires at least 18-24 months of treatment with medicines that are 100 times more expensive. This is because of added costs of hospitalisation, isolation precautions and expensive intravenous medications that may need to be given for two years or longer. The normal treatment for TB takes about six months. But if the dosage is not taken the way it should without a break, it may end up in MDRTB.
This treatment is quite toxic and often fails. MDRTB is caused by strains of the tuberculosis bacteria resistant to the two most effective anti-tuberculosis drugs available - isoniazid and rifampicin. MDRTB can only be diagnosed in a specialised laboratory. Unfortunately, reliable and representative data on the incidence rates of MDRTB in India is not available.
Bangalore-based Dr. P Anand, an allergy immunologist, has this to say: "I believe there is a lack of knowledge on the part of the doctors. Physicians need to be updated about the progress in the field. Patients are often given a lesser dose for a shorter period. Besides, hospitals tend to house resistant strains too."
Dr. Ramachandran points out that viruses do not recognise frontiers, and so we will soon have new strains for which we have no medicines to cure. For example, the deadly NIPAH virus distantly related to influenza that emanated from Malaysia was found in Siliguri, West Bengal. It was misunderstood for a variant form of measles leading to the death of several medical personnel.
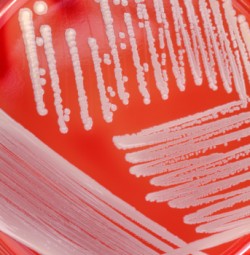
Methicillin-Resistant Staphylococcus Aureus (MRSA) is used to describe those examples of this organism that are resistant to commonly used antibiotics. Methicillin was a commonly used antibiotic to treat Staphylococcus aureus infections. It is now no longer used. The organism can easily be passed around by physical contact. MRSA organisms are usually found in hospitals. But it has also been found in the community. If MRSA organisms are passed on to someone who is already ill, then a more serious infection may occur in that individual. MRSA infections can cause a broad range of symptoms depending on the part of the body infected. These may be surgical wounds, eyes, skin and blood.
What is frightening is that patients with medical problems are now getting infected with MRSA after coming to the hospital. Invariably, you cannot prevent it in India, as hospital care is so poor in both government and municipal hospitals. But again, both these hospitals will say that there is no evidence to back it, as there is no centralized data.
Around three years ago, doctors at the Benaras Hindu University Institute of Medical Sciences in Varanasi found that strains of staphylococcus aureus bacteria seen on the skin and nostrils of healthy people had become resistant to antibiotics; these can cause life-threatening illness like pneumonia and septicemia. Though they found this only among two of the 783 samples taken from patients, it is enough to cause concern. Doctors said that it was the first vancomycin-resistant staphylococcus aureus (VRSA) strains from India.
India's battle with superbugs will be basically in the areas of diarroheal illness, respiratory diseases, malaria, filarial and of course, tuberculosis. "A good sewer system, elimination of open defecation, and provision of safe drinking water will help India contain 70 per cent of the infections," avers Dr. Ramachandran.
Dr Vipin Vashishtha, a consultant pediatrician in Bijnor, Uttar Pradesh, has seen numerous cases of drug resistant pneumoccocal meningitis. All his patients were resistant not only to penicillin but also to commonly used third generation cephalosporins like cefotaxime and ceftriaxone. Dr. Vashishtha says these drug resistant infections were earlier alien to India. However, he is not surprised. He says it was but natural for superbugs to arrive here, as there was a high use of inadvertent and irrational use of third generation cephalosporins and other newer antimicrobials in trivial infections that did not require such treatment - as in minor bronchitis, upper respiratory tract infections and diarrhea.
There are thousands of quacks operating as doctors in India especially in urban slums and rural areas that have poor health care. They merrily prescribe allopathic drugs that are not required, helping bacteria to learn how to grow resistant.
Educating doctors
In Pune, around 15 doctors from over a dozen hospitals meet once a month to discuss the dangers that superbugs pose to healthcare. Similar groups are active in Mumbai and other major cities. Says Dr. Vikram Padbidri, a microbiologist at the Jehangir Hospital in Pune, "We have to learn how to manage infection control. We cannot prevent the emergence of bacterial resistance, but we can control its spread. Doctors prescribe antibiotics carelessly. General Practioners need to be educated on its dangers and ensure that they judiciously prescribe it only when it is absolutely necessary."
The Artemis Health Institute at Gurgaon has put up posters where a patient is seen asking a doctor, "Have you washed your hands before examining me?" The hospital has put up hand sanitizers in the corridors and next to every bed to build up the culture of washing hands all the time.
A classic example of how infection control can be achieved is how Hong Kong dealt with SARS. There was no vaccine, there was no antibiotic. All that hospitals did was to practice infection control in every hospital very diligently.
Prof. S.K. Aggarwal, from the Department of Chest Diseases at the Banaras Hindu University, Varanasi, points out that in India, the failure to control infections by not completing the full course of drugs is very common, thus allowing most resistant microbes to survive, multiply and spread. Doctors feel that superbugs may make many existing antibiotics useless in another three to four years.
Today many drugs are becoming redundant as the bacteria has grown stronger than the drug. Many drugs at the research stage have been abandoned as it was found that the bacteria had already developed immunity to the drug. Stephen Palumbi, professor of Biology at Harvard University, says that in the face of rapid bacterial evolution, all drug strategies are temporary.
Superbugs will alter the course of medical history. It is one big challenge confronting doctors and drug companies today. In India, as elsewhere in the
world, there is a compelling need to put in place proper systems that will ensure that drug resistance does not set in. There has to be both biological
and social preparedness to meet the onslaught of drug resistant bacteria. It has to be done today, for tomorrow the bugs will be bigger and hungrier.